- Here we present highlights from a recent Biostime Nutrition webinar with guest speaker Karina Savage (BSc, BND, APD). Karina is a leading paediatric dietitian with 20 years’ clinical paediatric experience and is Director of the Smartbite Nutrition team (www.smartbite.com.au). Karina is a specialist in paediatric gut issues, including food allergies, intolerance, colic, IBS and IBD and coeliac disease.

As healthcare professionals, parents turn to us in their time of need for guidance and support around feeding their babies and young children. Providing them with key take home messages around feeding their children helps them feel more confident and empowered and can result in health benefits for their children. We need to tailor our key nutrition/ feeding messages based on the individual needs of that family.
We do this for the future health benefits of the child. Whilst a few key points may seem trivial, key nutrition suggestions could go a long way to optimising the health for that baby, reducing the risk of fussy eating, or preventing nutrient deficiencies. Ultimately, we are about helping parents to reduce the stress around feeding their little ones and giving parents confidence to help their children thrive.
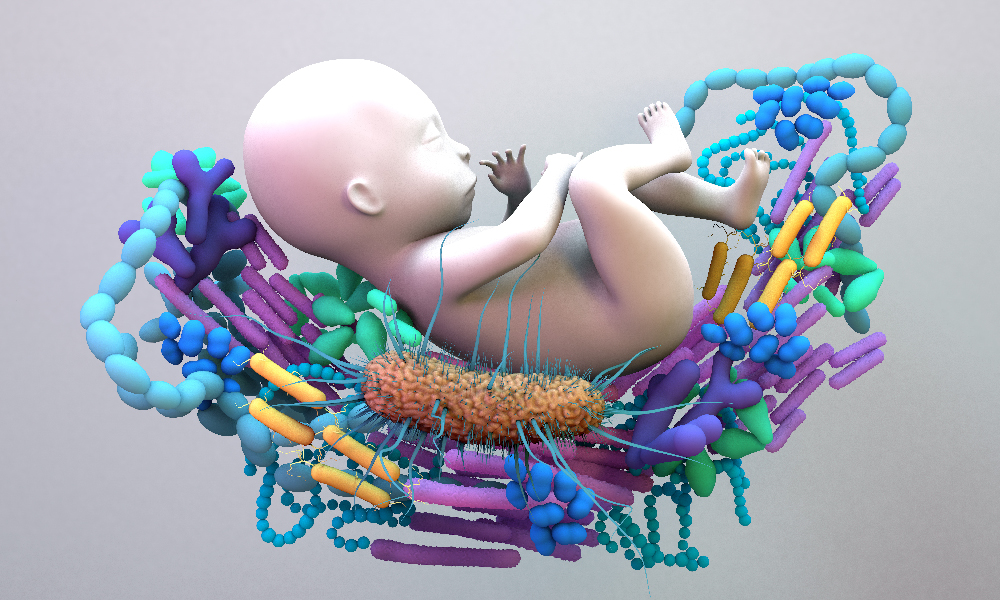
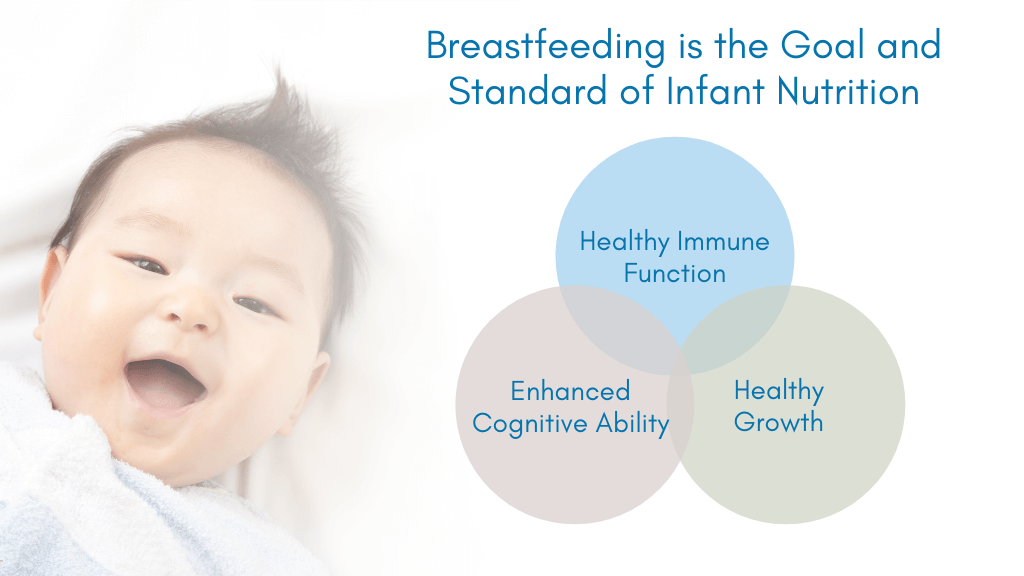
Optimising nutrition during the first 1000 days and beyond will certainly support gut health and the development of a robust immune system – one that is less likely to get sick or develop conditions, such as obesity or atopic disease. Summarised here are the key factors to consider when discussing nutrition strategies with parents.
Its relatively common knowledge that young children need at least 10–15 exposures to a new food before they necessarily accept it, however we need to better explain this phenomenon to parents. Babies have not had the same level of exposure to a food as adults have so we cannot expect them to always trust and eat a food straight away. As with every aspect of their life, it is a journey of development and exploration and food is no different. Learning about food is certainly a journey, and it is important we convey this to parents we speak to. Babies need to see, touch, smell and taste foods many times before they necessarily trust and eat it.
Young children need at least 10–15 exposures to a new food before they necessarily accept it.
The research tells us that 1/4 of parents of young children prematurely draw conclusions about their child’s preference for foods after 2 or less exposures. 1
This is understandable as a parent, however, this is where healthcare professionals can play a key role in supporting parents to continue with repeated exposures despite the food refusal. We need to give mums the motivation not to give up after the first few refusals, and to stay positive and in it for the long haul.
Children’s preferences and intake patterns are largely a reflection of the foods that become familiar to them.1 A greater variety of exposure to foods leads to a greater acceptance and broader intake of foods as the child develops. This makes sense because the child has a chance to learn about foods and to trust them over time (hopefully in a non-pressured environment).
When talking to parents, it is important to check their understanding of when to introduce allergenic foods (milk, soy, egg, wheat, fish and nuts). We need to encourage parents to introduce these foods by the age of 12 months to reduce the risk of the child developing a food allergy.2 The evidence is particularly strong for peanuts and eggs – both of which should ideally be introduced before the age of 12 months.3,4
Vitamin D deficiency may be a concern in Australia as we see significant levels of deficiency in winter particularly in the southern states.5 In many developed countries, there is also a suggestion of a rising incidence of rickets.6,7 Vitamin D is primarily obtained from sunlight exposure (ultraviolet B radiation) and historically only ~10% is attributed to dietary sources of vitamin D. However, when sun exposure is inadequate to maintain vitamin D status, dietary sources can make a small but useful contribution.
Vitamin D deficiency may be a concern in Australia as we are seeing significant levels of deficiency.5

Given the incidence of vitamin D deficiency we are now seeing, it may be sensible to start focussing more on obtaining vitamin D from food in the future to ensure sufficiency for future generations. Part of this strategy may well include the routine supplementation of all pregnant women and babies with 400 IU vitamin D daily.8 Practical strategies to increase dietary vitamin D intake include – consuming fish weekly, such as salmon, tuna, barramundi, basa, hoki and dory.
Other good sources of vitamin D (and choline) are eggs (specifically yolks). Mushrooms are also an excellent source of vitamin D2. The vitamin D content increases significantly if mushrooms are left out in the midday sun for 1–2 hours.9 Some margarines and butters are fortified with vitamin D, but many are not. The vitamin D content of many other Australian foods are currently unknown and need to be tested.10

Parents should not add sugar or honey to baby food as it increases the risk of dental caries and infant botulism (giving honey before 1 year is a risk factor for infant botulism).11 Another important reason for limiting all foods with added sugar is to reduce the likelihood of a child developing a “sweet tooth” which may lead to a preference for high sugar foods later in life.
Practical strategies include encouraging parents to avoid adding refined sugar to baby food or buying foods with added sugar. Instead sweeten baby food with fruit rather than sugar. All juice should be avoided unless a baby is constipated.
A good fibre intake when introducing solids supports a healthy gut mucosa and good bacterial diversity.13 If dietary fibre intake is insufficient, gut bacteria utilise mucus glycoproteins as a nutrient source, leading to erosion of the colonic mucus barrier. This compromises the integrity of the mucosal layer, which in turn can increase the risk of pathogens.
Good fibre intake when introducing solids supports a healthy gut mucosa and good bacterial diversity.13
For this reason, we need to encourage parents to give their babies fibre-rich plant foods at an early stage. Practical strategies include providing breads and cereals that are higher in wholegrains and oats. If possible keep the skin on fruit and vegetables (grating or pureeing into foods is fine). Nut butters and legumes are also great sources of dietary fibre to include regularly.
Salt should not be added to foods for infants. This is an important safety issue as infant kidneys are immature and unable to excrete excess salt.11
Instead, encourage parents to flavour baby food with herbs and spices, which will not only add flavour but are also rich sources of antioxidants.
To reduce the risk of iron deficiency in babies and young children, we need to encourage iron-containing foods as the first foods. This is important for neurocognitive development.

Iron-containing foods include iron-fortified cereals, meat and poultry, tofu and legumes. Care needs to be taken with a plant-based diet to ensure supplies of iron are adequate, as plant sources of iron are not as well absorbed.11 Pairing these foods with foods rich in vitamin C (such as citrus, rockmelon, strawberry, tomato, red capsicum and broccoli) will significantly improve the absorption of the non-haem iron.12
As healthcare professionals, we have the opportunity to make a big difference to the health of future generations. Keeping it simple, with three practical nutrition strategies that are specific to the family you are working with, will likely empower the parent and translate to health benefits for their child.
- Savage J, et al. J Law Med Ethics 2007;35(1):22–34 .
- Australasian Society of Clinical Immunology and Allergy (ASCIA). Parent Information: Frequently Asked Questions (FAQ) How to Introduce Solid Foods For Allergy Prevention .
- Du Toit G, et al. NEJM 2015;372:803–13 .
- Koplin JJ, et al. JACI Can early introduction of egg prevent egg allergy in infants? A population based study. October. 2010;126(4):P807–813 .
- Australian Health Survey: Biomedical Results for Nutrients (2011–12). Australian Bureau of Statistics .
- Robinson P, et al. Arch Dis Child 2006;91(7):564–8 .
- Thacher TD, et al. Mayo Clin Proc 2013;88(2):176–83 .
- Moon RJ, et al. Calcif Tissue Int 2020;106:30–46 .
- Cardwell G, et al. Nutrients 2018;10(10):1498 .
- Dunlop E, et al. Nutrients 2017;9(7):647 .
- Eat For Health – Infant Feeding Guidelines. Australian Government 2013 .
- Lane D and Richardson R. Free Radical Biology and Medicine. The active role of vitamin C in mammalian iron metabolism: Much more than just enhanced iron absorption. 2014;75:69–83 .
- Rodrıguez JM, et al. Microb Ecol Health Dis 2015;26:26050 .
- Desai MS, et al. Cell 2016;167(5):1339–53.e21 .
Are you a Healthcare Professional?
Important Notice and Declaration
Breast milk is best for babies. Professional advice should be followed before using an infant formula. Introducing partial bottle feeding could negatively affect breast feeding. Good maternal nutrition is important for breast feeding and reversing a decision not to breast feed may be difficult. Infant formula should always be used as directed. Proper use of an infant formula is important to the health of the infant. Social and financial implications should be considered when selecting a method of feeding.
The information provided on this website is intended for use by healthcare professionals only. It is a condition of use of this site that you are a healthcare professional within the meaning of regulations within your country of practice. Then denoting below Yes I am/No icons. For Healthcare Professionals based in Australia : It is a condition of use of this site that you are a healthcare professional within the meaning of the Marketing in Australia of Infant Formulas (MAIF) Agreement or the Therapeutic Goods Act.